13th September 2023
This instalment of our Healthcare Now series examines the label of ‘patient’ and we are so much more than this.
We joined our sister company, Bray Leino, to commission a nationwide healthcare study of over 1,000 respondents across both consumer and core patient groups – comprising those in primary care with an ongoing medical condition and those with a rare disease or unmet medical need. This exclusive quantitative and qualitative research study – Healthcare Now – unlocks invaluable insights which can guide us in understanding people’s attitudes and behaviours around healthcare and wellbeing, and which will help inform our approach to healthcare marketing.
We’ve all been a ‘patient’ at some point in our lives. This may have been a short-lived experience – perhaps you’re recalling that twenty-minute appointment you had with your GP about some symptom or other that cleared up after a few weeks. For others, being a patient may be a part of everyday life – maybe you were diagnosed with a chronic condition that now needs to be managed daily and reading this blog has reminded you that you’ve got a routine appointment coming up next week. No matter where you fall on the spectrum of ‘being a patient’, it’s not something that anyone should be reduced to. Afterall, you’re you… a complex human being who has been shaped by where you grew up, your cultural background, social roles, and life experiences… to name but a few aspects. Of course, being a patient may have contributed to who you’ve become, but that’s one piece of a larger, more complicated picture of who you are and your story.
Yet, in healthcare and the pharmaceutical industry, we’re guilty of committing this very crime: reducing patients to, or defining them by, their disease or condition. We spend so much time focussing on patients from a biomedical standpoint, that we forget that at the centre of healthcare are unique individuals who have diverse backgrounds and specific preferences, needs and abilities, all of which influence the way they approach their health and wellbeing.
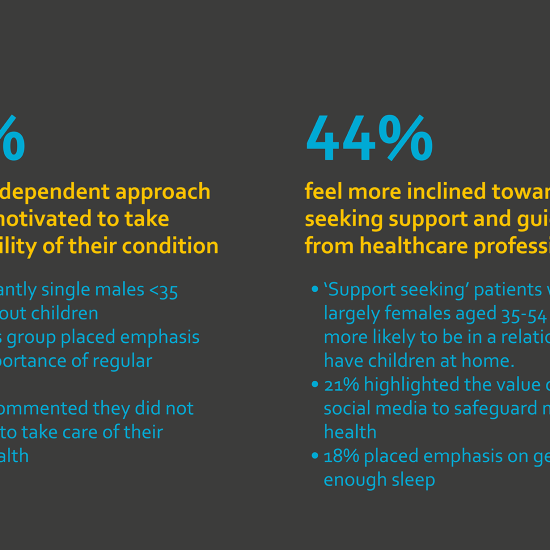
This very notion was echoed in our Healthcare Now survey which revealed that patients with long-term chronic conditions had an overall split in attitude towards how they manage their health and wellbeing.
Differing attitudes towards how we approach our health and wellbeing is hardly surprising – we all have our own perspectives. So why would that be different if you and I shared the same medical condition? Simply put, it wouldn’t.
For both healthcare professionals and the pharmaceutical industry alike, a cultural shift in how we communicate with patients is paramount to maximise value and benefit; meeting the vast range of patient needs, not just their medical needs. Not least of all, a shared medical label shouldn’t give rise to a generic communication style that doesn’t speak to the patient on a more personal level. Afterall, we are multi-dimensional beings, and a medical label is one of many components that contribute to a person’s overall identity.
Of course, shared perspectives can and do exist among patient groups, as illustrated by our findings showing that patients with long-term or chronic illness generally take a more proactive role across all areas:
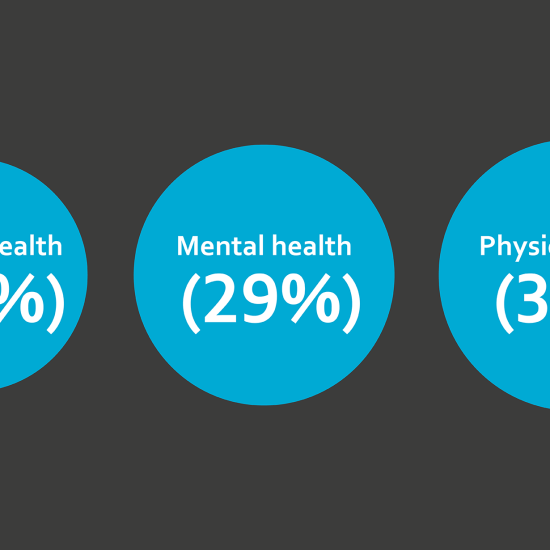
While shared perspectives and behaviours can help guide us in how we communicate with patient groups, it’s important to bear in mind that people are fundamentally unique with different expectations and priorities. Our Healthcare Now survey shed light on these nuances. We found that even though managing mental health is a common priority among patients living with a chronic illness, 22% of patients felt that no one would understand their health as well as they do, whereas 26% felt that healthcare professionals would understand the condition better than they do. It’s important we cater for the subtle, but fundamental, differences between each individual patient from the same patient group.
That’s not to say that an accurate diagnosis and knowing the name of their condition is not of the utmost importance for patients – particularly those with chronic, perhaps rare, yet undiagnosed conditions. An accurate diagnosis and a medical label are closely linked to a range of psychological benefits, restoring a sense of hope, and providing comfort. Patients often seek to share experiences on social media and benefit from a sense of community with those living with the same condition:
We’ll leave you to think back to the last time you communicated with a ‘patient’… did you see and treat them as a person first and foremost? Or did their medical condition dictate your manner of communication?
Klaus Sommer Paulsen, Founder of AdventureLAB and author of Integrated Storytelling by Design comments:
‘When we engage with people and become part of their lives in one form or another, we must remember a profound truth – or condition that will affect every moment of our shared time with them. Everyone lives their life narrative in which they have a leading role at the centre of the action and events. We use the accumulated life narrative – our experiences, beliefs, and understanding – as a filter to decipher and anticipate the world around us. In our starring role within, we strive forward as our trajectory builds our individual characters with every step as we move forward.
Or so it should be. But ever so often, the ideal design of things is just that – an ideal.
Our characters and, thus, identities are built through many defining moments. Sometimes we win, and sometimes we lose. Sometimes we make mistakes, and sometimes we learn from them. Undoubtedly, we’ve all made wrong choices and taken some wrong turns. However, most of the time the choices were still ours. We have a certain level of control throughout our lifelong storyline.
Imagine that control being taken away from you in an instant. Whatever influence you had on your own life narrative before, now you have significantly less. The level of control you thought you had was an ideal illusion.
With severe disease and diagnosis, you get forced down an uncertain path and through transformation of your self-image. The idea of what kind of story and role you were building for yourself is shattered. There may be hope, but from the onset of a condition, there is also doubt, fear and disbelief. How could this happen to me? These things always happen to someone else.
The disbelief and discomfort of the situation may turn into disconnection and distancing. In tumultuous situations, many cannot figure out the relationship between themselves and other characters in their lives, new and old. Do they care? For how long? Do they understand? Almost certainly not! With this kind of sentiment, it is no wonder that people seek the company of others who have been – or are going – through the same experiences as themselves. After all, by default, we are social animals, even though our life journey so far may have conditioned us otherwise. Here we are heard. Here we are seen. Nobody wants to be an extra without a voice in their own memoir.
So, what can we do to ensure that the person-turned-patient isn’t just seen as a diagnosis, with the accompanying lack of confidence in self and the capability to overcome? After all, transforming into something else can be challenging if you have become your diagnosis.
We must give everyone a voice and lend an ear to ensure they feel acknowledged.
Showing interest in individuals is vital to make a connection with them. As they open up and show who they are, you might find something in their past or personality – which are inevitably tied together – that can help them move forward. That which came before will tell you what has defined a person’s character and how they will adapt to this new, unfortunate chapter and role in their life narrative.
This may sound like yet another ideal, unachievable in a real-life, everyday setting. This is why new ways of thinking: dialogue over monologue, and life narrative over patient log must be part of the multi-faceted relationship with patients before, during, and after treatment. Sometimes, that means innovative ways of working within the organisation and with external partners to make sure the patient does not disappear in the shadow of their diagnosis. Luckily, quite a few principles and methods of designing and narrating scenarios which focus on, and empower, people lend themselves to healthcare to help achieve this. Actively pursuing this will add depth and value where the narratives of the person-turned-patient and the healthcare professionals overlap in a convergence that may very well be a healing factor in itself.
Storytelling in healthcare is not just reminiscing about what has happened, but influencing what will happen.’
Here at Solaris Health, we flourish in areas of unmet clinical need and would love to hear from you about your next challenge. Get in touch via hello@solarishealth.com or visit our website: https://solarishealth.com/
More information on AdventureLAB can be found at https://www.adventurelabstudio.com/